Focus on the progress of 2022WCLC and interpret research on NSCLC biomarkers
Author:Cancer Channel of the Medical Time:2022.08.13
*For medical professionals for reading reference

2022WCLC conference cutting edge courier, research progress!
The International Cancer Research Association (IASLC) World Lung Cancer Conference (WCLC) is an annual ceremony in the field of lung cancer. Many heavy research results are announced every year. The editor compiled and edited some research progress related to the biomarker of non-small cell lung cancer (NSCLC) on WCLC in 2022 [1-4] to readers.
Prediction of NSCLC's immunotherapy reaction through gene mutation features
(Summary number: MA05.03)
How to predict immunotherapy reactions is a problem that needs to be resolved in clinical urgent clinical. Researchers are exploring genetic mutations related to immunotherapy reactions and developed a genetic mutation -based risk model to better predict the clinical results of NSCLC immunotherapy.
Researchers collected 330 cases of NSCLC patients who received immunotherapy from the Study Cancer Center (MSK) queue research. Treatment NSCLC patients. Researchers choose genes with high mutation frequency and genes related to prognosis (P <0.05) for COX regression analysis. Based on these genes, researchers carry out Lasso return and establish prediction models. According to the calculation formula, the risk score of the sample is calculated, and the patients are divided into high -risk groups and low -risk groups according to the best critical value. The prognostic differences between the two groups of patients were analyzed by the Kaplan-Meier method.
The results showed that the researchers established a genome classifier composed of 6 decisive prognosis related genes used to calculate the risk score of patients with NSCLC: risk score = (0.395 × Keap1)-(0.384 × PTPRD) − (0.433 × EPHA3) (0.827 × EPHA5) − (1.253 × zfhx3) − (0.584 × mga)-(0.703 × NTRK3)+ (1.023 × PBRM1). According to the prediction model, tumor mutation load (TMB) of high -risk patients is low, and the immunotherapy response is poor. Kaplan-Meier analysis showed that the risk score and survival rate were negative (P <0.001). This study shows that the risk model based on gene mutations has been developed and proved to be the genome classifier of NSCLC, which can better predict immunotherapy reactions and may become potential indicators to guide immunotherapy decisions.
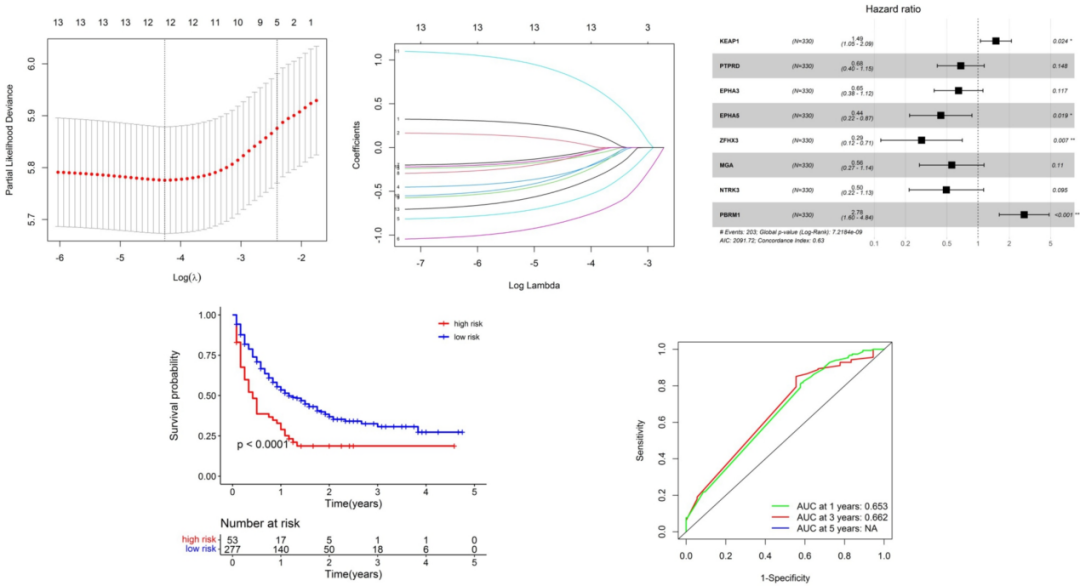
Figure 1. Analysis of patients with NSCLC patients

Figure 2. Analysis of patients with NSCLC
CREBBP as the potential biomarker of the immunotherapy of physical tumor and the correlation analysis of its immune microcyllar environment
(Summary number: MA05.05)
CREBBP gene guidance synthesize CREB binding protein, expressed extensively, and participates in the transcription of many different transcription factors. CREBBP directly regulates the DNA injury response (DDR) pathway, which is related to the occurrence of tumors and the efficacy of immune examination point inhibitors, but few clinical studies have confirmed this theory. A study analyzed the next -generation sequencing (NGS) data from the MSKCC research queue of 1661 patients and the Chinese clinical data of 14855 pantothena patients, and discussed the correlation between CREBBP mutations and immune biomarkers.
The results showed that 99 (59.6%) patients in the MSKCC queue carried CREBBP mutations, which was slightly higher than the Chinese queue (48.54%, 721/14855). In the MSKCC queue, the median tumor mutation load (TMB) of the CREBBP mutation group is higher than the wild group: 24.18 Muts/MB vs 6.26 Muts/MB, P <0.0001; Yuye Type: 39.08 Muts/MB VS 8.47 Muts/MB, P <0.0001.
Supplementary analysis shows that in the Chinese queue, there are significant differences between the microbesfast instability (MSI) (P <0.0001) and PD-L1 levels (P = 0.0019) between the CREBBP mutation group and the wild group. In terms of prognosis of immunotherapy, CREBBP mutations are significantly related to the median total survival (OS) of bladder cancer, colorectal cancer, and NSCLC. NR, HR = 0.42, P = 0.017; 43 months VS 13 months, HR = 0.23, P = 0.0085; 4.8 months vs 13.5 months, HR = 2.04, P = 0.00084. In NSCLC, CREBBP mutations are negatively related to the efficacy of immunotherapy. Study the correlation between CREBBP and immune microcontinoma, and found that CD4+ T cells and NK cells in bladder cancer and colorectal cancer have significantly increased significantly, but it is significantly reduced in NSCLC, which may be the opposite cause of the prognosis.
The study shows that CREBBP has a high correlation with TMB, MSI, and PD-L1 in solid tumors. CREBBP may be potential biomarkers for immunotherapy, and immune microe environmental may be a factor affecting CREBBP. Through the history of specific mutations, historical and smoking, study NSCLC's MET14 outer Xianzi jump mutation mutation
(Summary number: MA05.08)
Although MET14 external jumping and mutations are common in lung adenocarcinoma (LUAD), unlike other common driving genes, it is also found in patients with squamous carcinoma and smoking history. A study adopts the tissue sample of NGS -based NGS, all -exogenous sub -group sequencing, RNA -based full transcription group sequencing or immunohistochemical analysis of NSCLC patients. The correlation between history and mutations.
In 440 NSCLC samples containing MET14 out -of -the -art sub -jump mutations, 147 different mutations were found, and more than 11 protein changes were found. The most common MET14 out -of -the -art sub -jump jumps are: D1028H (8.4%), D1028N (7.0%), C.3082+2T & C (5.7%), D1028Y (5.2%), C.3082+1G & A (4.5%). TP53 mutations are more common (43.9%), but it will change the jumping mutation of outsiders No. 14, which will be changed; 53.9%C.3082+3A & T patients have TP53 common mutations, while C.3082+1G & T only has only in C.3082+1G & T. 21.1%exists in TP53 mutations. Among all MET No. 14 out -of -the -mall jump mutation cases, 8.6%are highly expressed tumor mutation load (TMB). 82.2%of MET No. 14 outer appendal jump mutation sample PD-L1 expression ≥1%, but this situation also changed from mutation, Met C.3082+1G & C's median PD-L1 tumor ratio score (TPS) was 97.5 %, Met C.3082+3A & G's median TPS is 0%(Q <0.05).
49 cases (11.1%) are squamous carcinoma tissues, 381 cases (86.6%) are non -squamous tissues, and 10 (0.2%) are gonadocyroma tissue. TP53 mutations are more common in MET No. 14 outer Xianzi jumping scales carcinoma tissue (90.4%) than MET No. 14 outer Xianzi jump mutant non -scale carcinoma tissue (60.7%). The median OS of patients with outer outer outer jumping outer outer outer jumping and mutagenic squamous carcinoma is shorter than those of non -squamous carcinoma (336 vs. 1106 days, HR 1.22, P = 0.47). Nine3 patients with Met 14 Excerpts of Xianzi jumping mutations can evaluate the smoking status, 79 of which (84.9%) are smokers, and 14 (15.1%) are non -smokers. Compared with smokers, non-smokers HLA-G (TPM) MRNA expression significantly increased (0.31 vs. 0.09 TPM, Q <0.05).
The study shows that in different MET No. 14 out-of-reveal jump mutations, there are heterogeneity, TMB and PD-L1 expressions. MET No. 14 outer sub -jump mutations occur in the scale and non -scale NSCLC, but there are differences in co -mutations and organizational results. Compared with non-smokers, the HLA-G mRNA expression of smokers is low. The impact of these differences on treatment is worth further studies.
Genetic positioning of organ metastasis: analysis of 2326 cases of primary pulmonary adenocarcinoma and organ specific metastasis
(Summary number: MA05.09)
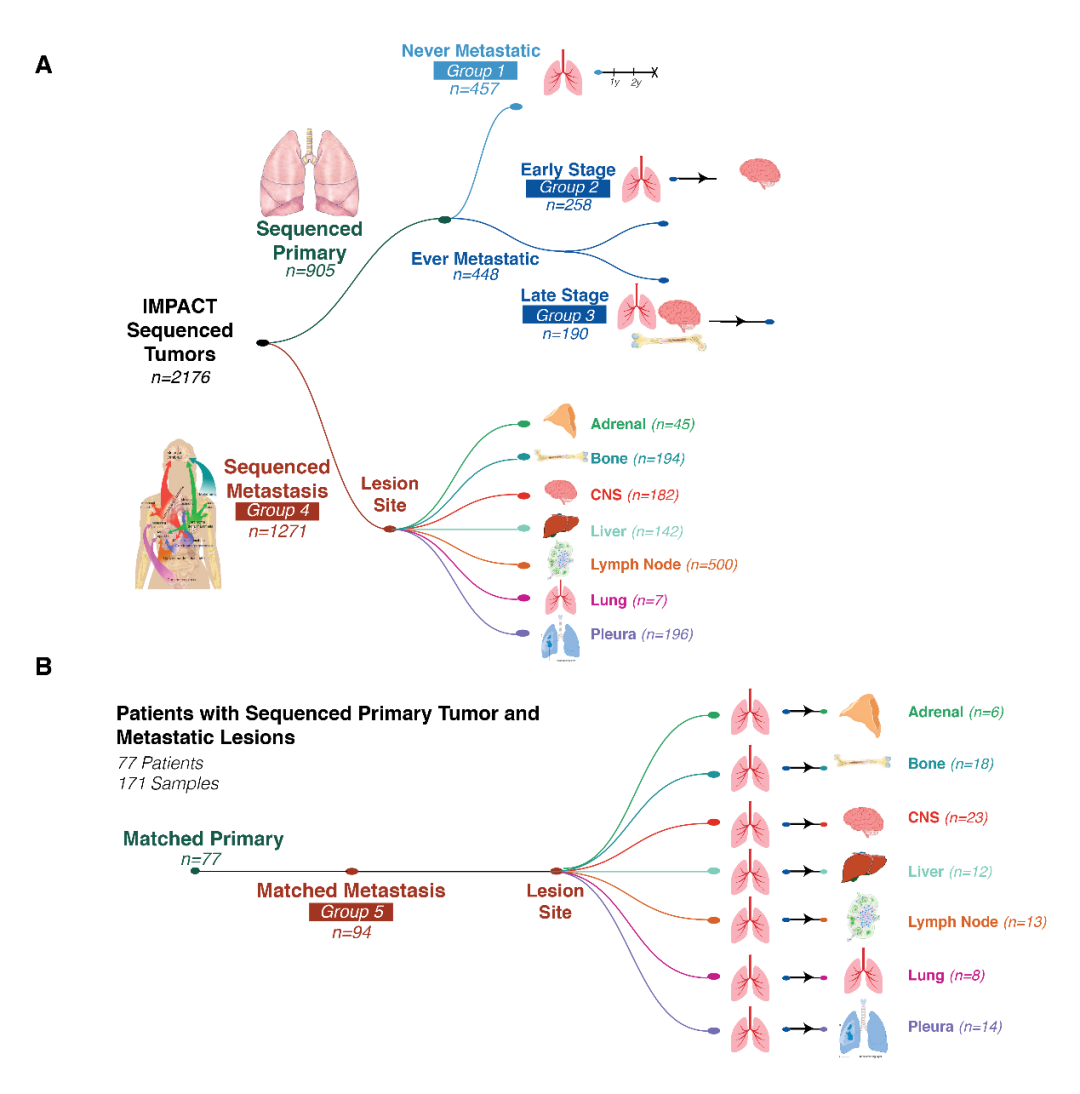
Pulmonary adenocarcinoma (LUAD) is preferentially metastasized to a specific organs, which is called organ affinity. A study conducted a comprehensive analysis of the clinical pathological and genome data of a single institution to determine the characteristics related to LUAD transfer and organ affinity. Researchers checked 2326 LUAD samples with clinical pathological annotations and broad -spectrum NGS genome data. The history of metastasis is drawn into 7 common organs, including adrenal glands, skeletal, central nervous system (CNS), liver, lung, lymph nodes (LN) and pleural.
The analysis found that the clinical pathology and genomes related to metastatic tumors were determined, including 4 genes (EGFR, MYC, SMARCA4, and TP53), which were also related to non -metastatic survival (MFS). In the characteristics related to metastatic tumors, young, male, TP53 changes and ERBB2 changes are also related to greater metastasis. In the analysis of specific transfer of parts, the SMARCA4 and TP53 mutations are related to the organs of bones and LN, respectively. CDKN2A changes and HIPPO pathway changes have short bone metastasis and CNS transfer time, respectively. Studies have shown that compared with primary tumors, the tumor mutation load (TMB) of metastlasia tumors is higher, and the chromosomes are more unstable, but there is no corresponding treatment target.
Figure 3. Primary stove and transfer stove drawing
This material is supported by Astrikon, for medical professionals for reference
Approval number: CN-100365 Expired Date: 2023-8-4 References:
[1] xiaoxuan wu, peng song, jianming ying, et al. MA05.03 -Utilization of geenomic mutation signature to predict the immunotherapy response in non -Small Cell LUNGACER. 2022WCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLCLA.
[2] Xue Hu, Yating Zheng. Analysis of Crebbp as a Potential Biomarker for Immune Checkpoint Therapy in Solid Tumors and ITS CORRELELATH Immune Microenvironmet. 2022W22WCL.5555555555555555555555555555555555555555555ORO
[4] Harry Leengel. Genomic Mapping of Metastatic Organotropism: Analysis of 2326 Primary and Organ-Spectastases in LUNG ADENOCARCINOMA. 2022WCLC. MA05.09.
*This article is only used to provide scientific information to medical people, and does not represent the viewpoint of this platform

- END -
Do 6 things a good day every day, the skin will really be younger
Beijing Tiantan HospitalPublic account ID: Tiantanhospitalfocus onSpecialist Jian ...
After the family's trivial matters were furious, the man had a sudden aorta clay layer

Jimu Journalist Liao ShiqiVideo editing Zhang JianCorrespondent Ma Yaoyao