Unknown causes of severe acute hepatitis diagnosis and treatment guidelines (trial)
Author:China Centers for Disease Cont Time:2022.06.17
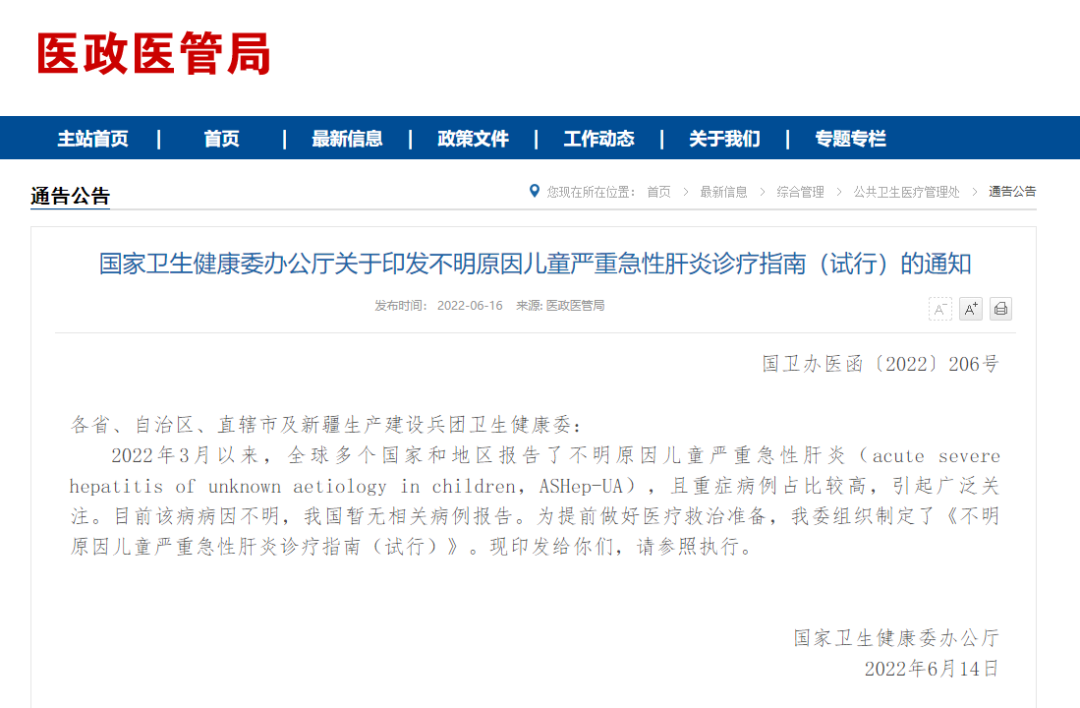
Unknown causes of severe acute hepatitis diagnosis and treatment guidelines
(Trial)
On March 31, 2022, for the first time in the Scottish region of the United Kingdom, children's serious acute hepatitis (ASHEP-UA), such as an Acute Severe Hepatitis of UNKNOWN AEETIOLOGY in Children. High, causing widespread attention. Since April 12, 2022, the European Disease Control and Prevention and Control Center and the World Health Organization (WHO) official website have repeatedly announced this disease -related information. On April 23, 2022, WHO issued a diagnostic suggestion, but because of the unknown cause, there was no recommendation on the treatment plan. There are no relevant case reports in my country. In order to effectively strengthen the early identification and standard diagnosis and treatment of the disease, and make every effort to improve the treatment effect, our committee will form a "Guidelines for the Diagnosis and Treatment of Severe Acute Hepatitis for Children (Trial)" based on relevant reports and literature and literature.
1. Popular overview
On March 31, 2022, five children in the United Kingdom reported that five children had severe hepatitis within 3 weeks, and children were 3 to 5 years old. On April 5, 2022, the United Kingdom reported to WHO that the unknown cause of acute hepatitis in healthy children under 10 years of age increased. Children had vomiting, jaundice, and high -rise aminase. As of May 20, 2022, the European monitoring system data shows that the disease can be seen in children at all ages, which are more common under 5 years of age; 14.1%of inpatient children need to live in severe care ward. On May 27, 2022, WHO announced that 33 countries reported 650 suspected cases, at least 38 cases of liver transplantation, and 9 deaths.
There is no obvious epidemiological association between various cases, and it does not support it as a contagious disease.
Second, cause and pathogenesis mechanism
The cause and pathogenesis of serious acute hepatitis in children are still studying. At present, WHO believes that although the hypothesis of adenovirus infection as the cause of the cause has a certain rationality, adenovirus usually causes a mild and self -limiting digestive or respiratory infection of children with low age, which cannot fully explain the more serious clinical manifestations of the disease. Therefore, the correlation between the disease and the adenovirus needs to be further clarified. Most children have not been vaccinated with new coronal virus vaccines and do not support hypothesis related to the side effects of the new coronal virus vaccine. Other pathogenic factors are still exploring. For example, during the popularity of new coronary pneumonia, the level of adenovirus is low, which increases children's susceptibility; new adenovirus occurs; adenovirus combined with new coronal virus infection; new coronal virus infection complications lead to super antigen media media Immune cells activated, which causes children's multi -system inflammatory syndrome. The exploration of other pathogens is also underway, and non -infectious factors also need to be eliminated.
3. Clinical manifestations
Acute onset, mostly manifestations of dysfunction, nausea, vomiting, diarrhea, abdominal pain and other digestive tract symptoms, followed by yellow red red, skin and scleral yellow stains, and some children may have a white stool color, liver swelling, and liver swelling Symptoms of heat, fever and respiratory tract, individual may have spleen enlarged. A small number of cases can progress in a short period of time to acute liver failure, and jaundice has performed aggravation and hepatic encephalopathy.
Fourth, case definition
(1) Suspected of cases: From October 1, 2021, with acute hepatitis (non -A, B, C, Ding, Pantharitis) and serum to 500 IU/L (ALT or AST), the age is 16 The age and below.
(2) Cases of epidemiological associations: Starting from October 1, 2021, acute hepatitis (non -A, B, C, Ding, and penta hepatitis) who are closely contacted with suspected cases.
(3) There are currently no diagnostic standards for diagnosis.
Suspected cases and epidemiological associations must pay attention to eliminating hepatitis, common non -hepatitis virus infections (such as EB virus, giant cyt virus, etc.), autoimmune diseases, and genetic metabolic diseases.
Fifth, diagnosis of acute liver failure
Suspected cases or epidemiological associated cases meet the following three criteria:
1. The liver disease of acute attacks has no evidence of chronic liver disease;
2. Evidence of biochemical evidence of severe liver injury;
3. Abnormal coagulation that can not be corrected by vitamin K, and meets one of the following two: (1) The original time (PT) ≥15s or international standard ratio (INR) ≥1.5, accompanied by hepatic encephalopathy; (2) PT ≥ PT ≥ PT ≥ 20s or INR ≥ 2, accompanied by hepatic brain disease.
6. Laboratory inspection
The following laboratory examination is performed according to the needs of the condition to assist in clarifying the cause and judgment of the condition.
(1) Conventional inspection. Blood routine and mesh weaving red blood cells, C -reactive protein, calcium calcium original and urine, routine and other indicators.
(2) Biochemical examination.
1. Liver function: Alanine aminotransferase (ALT), citizen amino aminotransome (AST), total bilirubin and direct bilirubin, albumin, alkaline phosphatase, γ-glutamyl metastasis Enzyme, bile acid, etc.
2. Other: hemogenous, blood glucose, lactic acid, blood ammonia, renal function, myocardial enzyme spectrum, etc.
(3) Coagulation function examination. PT, coagulantogenic activity, INR, and activated coagulant time time.
(4) pathogenic examination. In the case of except for the infection of foreign A, B, C, Ding, and pentitis virus infection, multiple samples should be left as much as possible for the cause survey, including blood (whole blood and plasma), respiratory tract (nasopharynx or oral pharyngeal wipe Zi, nasopharyngeal absorbing objects, etc.), feces and urine samples. If you need to be punctured clinically, tissue samples can be saved. It is recommended to give priority to the following original disease examination. In unconditional testing, the specimen should be actively collected and the preparation should be preserved properly.
1. Nucleic acid detection: The suitable specimen is blood, respiratory tract or tissue samples. Those with conditions should try to complete the new coronary virus, giant cyt virus, EB virus, human herpes virus 6, human intestinal virus (universal type of enterovirus) Virus, adenovirus (note that the adenovirus type that can be tested by reagents should be tested as much as possible including virus nucleic acid tests such as virus type 40/41) and small virus type B19; those with gastrointestinal symptoms such as vomit Nucleic acid testing such as viruses, wheel viruses and Noro viruses.
2. antigen test: Those with gastrointestinal symptoms such as vomiting and diarrhea can perform antigen tests such as adenovirus, rotary virus, and norvir virus in the stool specimen.
3. Serum specific antibody detection: Those with conditions try to complete virus specific IgM and IGG detection of viruses such as new coronary virus, EB virus, giant cell virus, small virus B19, and herpes simplex virus.
4. Those who are negative and highly suspected clinical infection can be checked in the above -mentioned diseases. Samples such as blood and liver puncture tissue can be sequensed.
(5) Other inspections. Poison screening, drug testing, immune function test, autoimmune antibody examination, and genetic metabolic disease screening can be performed according to clinical diagnosis and treatment needs.
(6) Liver puncture biopsy. According to the needs of the disease, it is necessary to determine whether the liver puncture biopsy is performed, and the biopsy can be performed for pathological and pathological examinations.
Seven, imaging performance
(1) Abdominal ultrasound. Suggestion first choice. Ultrasonic examination can be used to evaluate the liver size, contour, hardness, liver substantial echo, gallbladder and ascites, etc., and can also be used as evaluation methods before liver transplantation.
(2) MRI in the abdomen. You can choose according to the situation of the child as appropriate.
8. Treatment measures
Comprehensive treatment measures focusing on the symptoms and supporting treatment should be taken, and the condition changes should be observed closely, the mental state should be evaluated, the laboratory indicators are monitored, and complications are prevented. Patients with liver failure should be referred to hospitals with ability to treat.
(1) Treatment of hepatitis.
1. General treatment and care:
(1) Rest: Reduce physical consumption and avoid strenuous exercise; when jaundice, vomiting, fatigue, and difference, you should rest properly.
(2) Nutritional support: ensure calorie intake, give high carbohydrates, low -fat, and high -quality protein diets for children who can eat, and supplement a variety of vitamins. Those with insufficient eating need to supplement veins.
(3) Monitor the changes in the condition, and actively correct low albumin lenin, hypoglycemia, hydrolysis, and acid -base balance disorders, and be alert to complications such as liver failure.
2. Symptoms: Select liver care drugs as appropriate. Those with bile stasis can use bear to remove oxygenic acid; pay attention to keeping stools smoothly. Those with constipation can use lactose sugar to reduce poison absorption.
(2) Liver failure treatment.
Can be transferred to the intensive care unit and give life support treatment under strict guardianship. The close collaboration of multi -disciplinary teams helps to increase the survival rate of patients.
1. Liquid treatment: The total intravenous infusion should be limited to avoid using liquid -containing liquid, adjust the glucose injection rate according to the blood glucose level, maintain the electrolyte balance, and pay attention to correcting low albumin lesy. If the cycle appears unstable, the liquid recovery should be given.
2. Hepatogenous encephalopathy and intracranial hypertension: keep the environment quiet; reduce unnecessary stimuli; use sedative drugs with caution; timely discover and treatment of factors that may increase the condition, including infection, shock, digestive tract bleeding, acute kidney injury and water Electrolytic disorders, etc.; Those with cerebral edema, intracranial hypertension can be given glycol, hypertonous saline and diuretics.
3. Hypelemia: When blood ammonia is significantly elevated or accompanied by hepatic encephalopathy, the protein intake should be reduced to 1g/kg/d; giving it or high -level enema to promote defecation in oral or high -level enema, reducing the intestinal ammonia in the intestinal tract. Absorption; venous infusion of arginine, permine-birdine, etc. to promote ammonia excretion; use branches of amino acid as appropriate. If it is still invalid or the blood ammonia is severely increased, blood purification therapy should be considered.
4. Coagulation dysfunction: Vitamin K1 with veins; supplement fresh frozen plasma and/or platelets when there are active bleeding or invasive operations, decreased fibrinogen (<1g/L) to be cold sediment; if no active bleeding Or invasive operations, it is not recommended to give blood products to correct the abnormal coagulation to avoid adverse reactions such as transfusion such as liquid overload.
5. Respiratory failure: If the nasal duct is absorbed by the hypoxia, the nasal duct absorption is still not relieved or aggravated, and the non -invasive or invasive ventilation is as appropriate.
6. Cardiovascular dysfunction: Maintain effective circulating blood capacity; those with reduced blood pressure, obstacles of cardiac functional disorders can be increased and hearty -hearted drugs can maintain proper blood pressure and improve myocardial contraction.
7. Acute renal injury: Reduce or discontinue diuretics to avoid using kidney toxic drugs and maintain effective blood capacity. Those with low blood pressure can be used to infusion of Telicin or norepinephrine combined with albumin. After the treatment of drugs, there are still severe urine or urine -free, hydraulic overload, elevated serum creatinine, severe electrolyte and acid -base balance disorders.
8. Control secondary infection: When a secondary infection is suspected, antibacterial drug treatment should be started after leaving related pathogenic specimens. After the pathogen is clear, it should be adjusted in time according to the training and drug sensitivity results. 9. External liver support treatment: It is mainly used for severe coagulation abnormalities, hepatic encephalopathy, etc. that cannot be relieved, or as transitional therapy before liver transplantation. You can choose plasma replacement, blood irrigation and plasma adsorption.
10. Liver transplantation: Patients with severe liver failure who are invalid in the treatment of internal medicine should organize multidisciplinary team evaluation as soon as possible to decide whether to transplant liver transplantation.
Nine, prevention and control measures
(1) Strengthen hand hygiene, pay attention to wearing masks and diet hygiene.
(2) In clinical work, medical staff must take standard prevention measures. Once a suspected case is found, it should be reported in time in accordance with the requirements.
(Source: Official Website of the National Health Commission)
- END -
As soon as it arrives, it will become a "big oil field"!Where did the oil from the nose come from?

I believe many people have had the trouble of nose out of oilEspecially at present...
Liu Lin Police Station deeply carried out the prevention and control of hotel epidemic in the jurisd

In order to effectively do a good job of preventing and controlling and safe busi...