New discovery!The internal immune system of the brain is stronger than expected
Author:Cool brain Time:2022.09.20

Via: pixabay
The following is the audio of the full text of Miss Sister
Author | Diana Kwon
Translation | Caroline
Grade -Cool Brain Creative
Reading | Pigeon Tsai
Artist | Jenny
Edit | Sales increase
The defense of the brain has its own walls and defense, and its border has active immune cells busy.
The brain is the master of the body and is protected by the lofty status. The cells have long cell life and refuge in a "defense facility" called a blood -brain barrier. For a long time, scientists believe that the brain is completely isolated from the other parts of the body -especially the differences between the two defense systems. When a large number of immune cells fight against the other part of the body, the action may threaten the brain's dilemma.
However, in the past ten years, scientists have found that the work of protecting the brain is not as simple as they imagine. They learned that the brain's defense workers have their own walls and defense, and their borders have active immune cells busy.
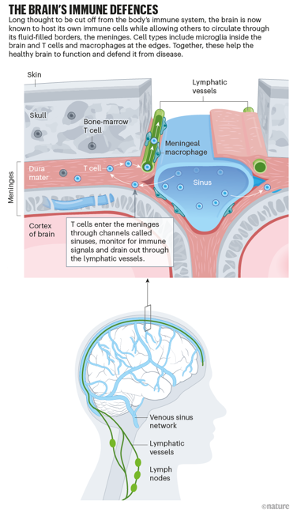
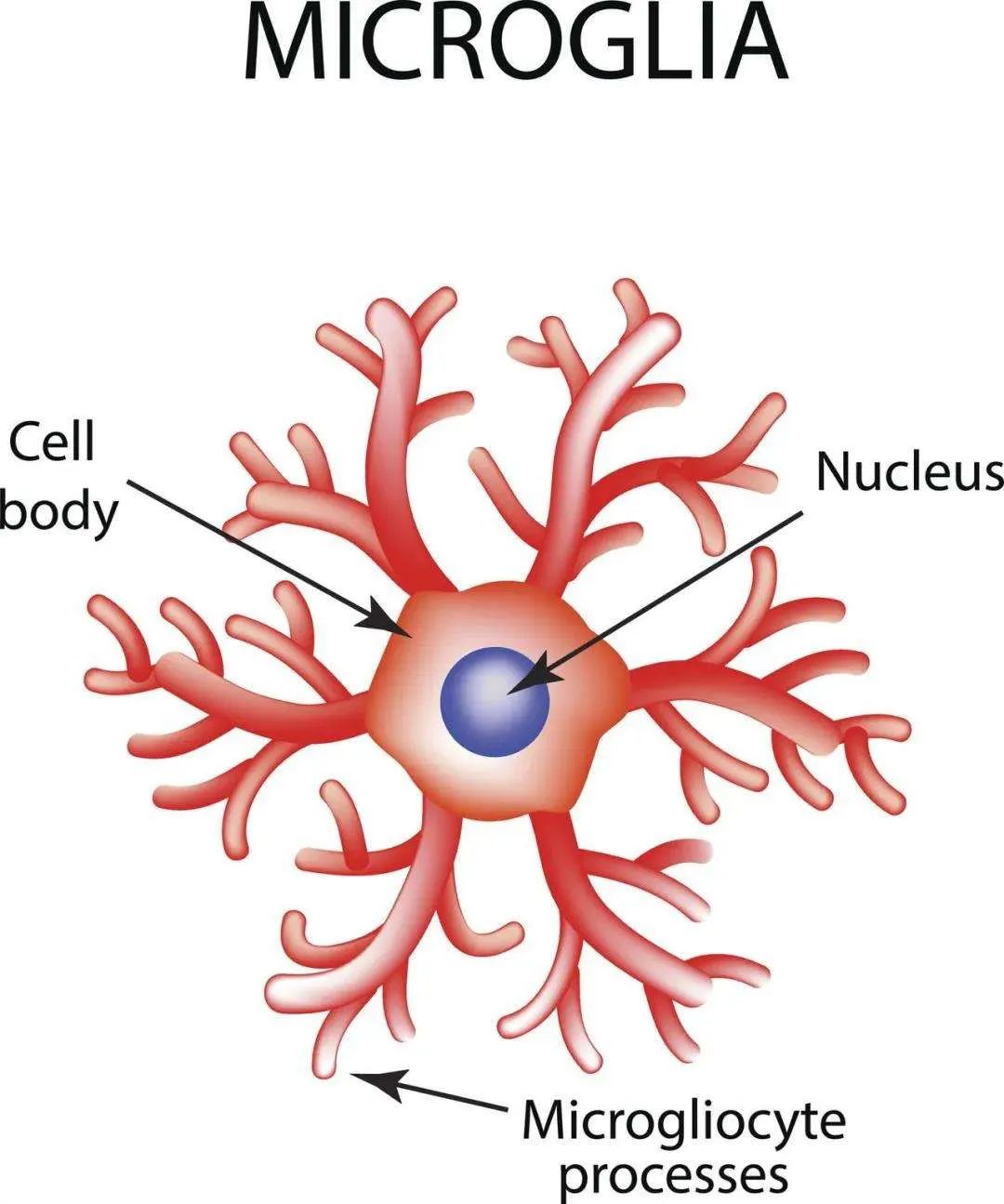
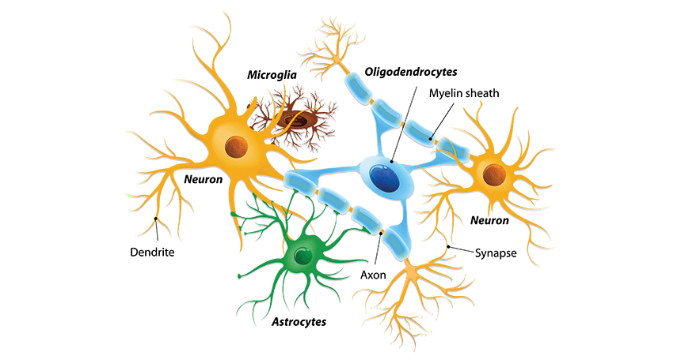
A large number of evidence now shows that the brain and the immune system are closely linked. Scientists already know that the brain has its own permanent immunoconon, called small glue cells. Recent discovery depicts more detailed pictures for their functions and reveals the characteristics of other immunoles stationed in the area around the brain. Some of these cells come from other parts of the body, and some are produced in the bone marrow. By studying these immune cells and drawing their interactive diagrams with the brain, researchers have found that they play an important role in healthy, ill or damaged brains.
Scientists no longer think that the brain is a special, closed area. Kiavash Movahdi, a neurotomian at the University of Brussels Liberty, said: "The idea of the brain's immune privilege is now quite outdated." He added that although the brain is still regarded as a unique area in immunology, Because its barrier prevents immune cells from entering and leaving at will. But it is obvious that the brain and immune system are in continuous interaction.
Via: Nik Spencer/Nature
Leonardo Ternelli, head of the State Institute of Mental Health, said that the transformation of this attitude towards the brain is common in society. Almost every neuroscience accepted this kind of connect. Although many people still need to catch up with the latest discovery of neuromanological, these discoveries have begun to reveal the potential mechanism of the brain.
Tony Visi at Stanford University in California said that people are eager to understand how the brain and immune system are combined, and whether this connection will affect normal brain function or there is a certain importance in diseases. But this is currently a very difficult question.
Privilege space
Twenty years ago, when neuromatologist Mihar Schwartz just established her laboratory in the Institute of Science in Requesman in Israel, she couldn't help asking herself a question: the brain: the brain Is it really true with immune protection? Is this really true? She said: "The brain cannot tolerate any immune activity. It is completely self -evident. At that time, everyone thought that if there was any immune activation in your brain, it was a sign of pathology." However, it is indispensable like the brain. Organization cannot enjoy the benefits of immune system assistance, which is actually unreasonable.
The idea of the restricted area of the immune system has taken root as early as decades ago. As early as the 1920s, Japanese scientist Baijing reported that when tumor cells were implanted in rats, the immune response destroyed it; The immune response is weak or lacking. Similar discoveries also appeared in the 1940s.
Most scientists also believe that the brain lacks a system that transports immunomaste in and out. At that time, the mainstream view was that the brain and the immune system were largely separated, and the two would only have contact with the situation of hostile: when immune cell rebellion, attacking the human body's own cells in diseases such as multiple sclerosis and other diseases such as multiple sclerosis diseases and other diseases Time.
Therefore, in the end of the 1990s, when Schwartz and her team reported that after the central nervous system was acute, two types of immune cells (macrophages and T cells) were protected from damage to the neurons. Many scientists doubt when they support their recovery. Schwartz recalled: "Everyone at the time told me that your discovery must be wrong."
Since those early experiments, Schwartz's team has accumulated a lot of evidence, indicating that immune cells have indeed played an important role in the brain, even if there is no autoimmune disease. For example, researchers have shown that among mice that lack the immune system, neurodegenerative diseases, such as motor neuronal diseases (muscle atrophic spinal cord side sclerosis) and Alzheimer's disease, seem to progress faster, The restoration of the immune system slows their progress. Scientists have also revealed the potential role of small glue cells in Alzheimer's disease.
Recently, scientists have stated that immune cells on the edge of the brain are active in neurodegenerative diseases. After checking the cerebrospinal fluid of Alzheimer's patients, Tony Vis and his colleagues found evidence that the number of T cells increased by the border of the brain full of liquid. Tony Vis said that the expansion of these immune cell groups indicates that they may play a role in the disease. But whether immune cells hurt the brain or help, it is still unreasonable. In the study of Alzheimer's disease and other neurotic diseases, Tony Vis and his colleagues believe that the immune system may damage neurons by releasing molecules that promote inflammation and trigger cell death. Others proposed that T cells and other immune cells may be protected. For example, Schwartz's research team reported that in the mice model of Alzheimer's disease, improving immune response can cause the removal of starch -like plaques and improve cognitive capabilities.
Brain system structure
Busy border
What is more and more clear now is that the edge of the brain is a variety of immunology: almost all types of immune cells in the body can be found in the area around the brain. Movakdi said that the meninge is a "immunology fairyland", which happened too much.
In 2021, Jonathan Kipneis, a neurotomian at the University of Washington, reported that there is a local source of immune cells: the bone marrow of the skull.
When they explore how the bone marrow mobilizes these cells, Kipneis proves that the signal carried in the cerebrospinal fluid is passed to the cranial bone marrow in the case of damage to the central nervous system or the pathogens, prompting it to produce and release these cells.
With the accumulation of evidence that immune cells participated during brain injury and disease, researchers have been exploring their functions in the healthy brain. "The neuroscience at the Boston Children's Hospital Beth Stevens said:" I think the most exciting part of neuromanological is related to many different diseases and conditions and normal physiological physiology.
Many research teams including Stevens have found that small gel cells are important to brain development. These cells participated in the trimming neuron connection. Studies have shown that problems in the pruning process may lead to neurological development.
Border immune cells have also been proven to be essential in a healthy brain. For example, Kipneis, Schwartz, and their teams have proven that mice who lack these cells show problems in learning and social behavior. Others reported in 2020 that there were no mice in the brain and other parts of the body, and there were defective small glue cells. Their small gel cells worked hard to trim neurons during development, leading to excessive synapses and abnormal behaviors. During this critical period, T cells migrated to the brain and helped mature small gel cells.
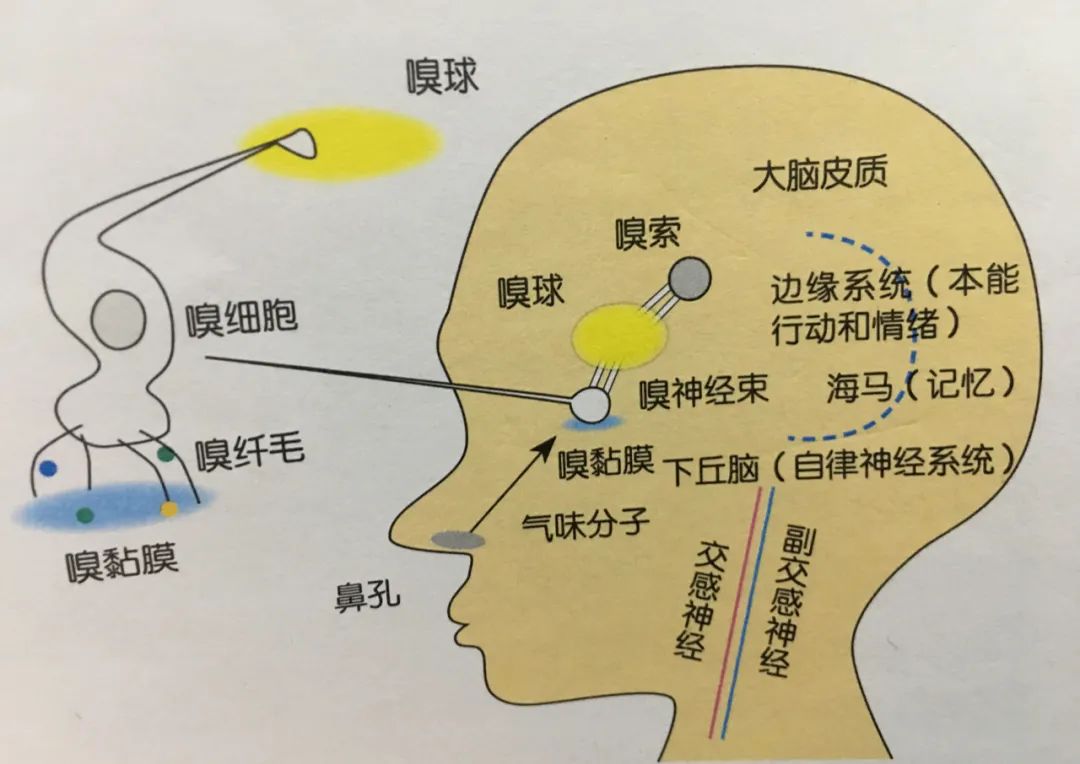
A big mystery is immune cells, especially how immune cells around the border are talking to the brain. Although there are some evidence that they may occasionally enter the brain, most studies so far show that these cells communicate by sending molecular messes called cytokines.
Researchers have been studying how cytokines affect their behavior for decades. For example, cytokines that immune cells emit during infection can start "disease behavior", such as adding sleep. They are also displayed in animal models that changes in cytokines can lead to changes in memory, learning and social behavior. At present, how cytokines enter the brain and play their role are still a field of positive research.
Cyclicals may also be a connection between the immune system and the neuros development (such as autism). When the neurotomian Cai Cai and her colleagues at the Massachusetts Institute of Technology, the University of Massachusettons of Cambridge improved the levels of cellular factor of pregnant mice, they saw the brain changes and similar behaviors of future generations.
Although these insights are seductive, many tasks about immune cells, especially the boundary of immune cells in the brain are still in its infancy. Kip Nice said: "We are still far from understanding the real situation in the brain."
a
Two -way channel
The exchanges between the immune system and the brain also seem to have another direction: the brain can guide the immune system.
Some of these opinions were available decades ago. In the 1970s, scientists combined with sugar essence (an artificial sweetener) with an immunosuppressive drug for several days, so that the rats had immunosuppressive when tasting sugar.
In the recent work, the neuromanosterist of the Israeli Institute of Technology, Asia Rose, and her team discussed the relationship between mice, immunity and cancer. They reported in 2018 that the neurons that activated the covered area of the abdomen, a brain area involving positive emotions and motivations, promoted immune response, in turn, and slowed the growth of tumors.
Then, in 2021, Rose determined the neuron of the island -like cortex -one part of the brain, involving emotional and physical sensation -it was active during colon inflammation, and this situation was also called colitis.
Through artificially activating these neurons, researchers can regain the intestinal immune response. Just as Pavlov's dog learned to connect the sound of the bell with food, so that the animals would drool at any time. Restart. "This indicates that there is a very strong string between neurons and immune cells." Ross suspected that the bio -immune "memory" was favorable, because they were favorable, and they might encounters the body and encountered it in the body. In the case of pathogens, prepare the immune system. She added that in some cases, they may not adapt to: when the body foresees infection and makes unnecessary immune reactions, it will cause damage. Rose said this approach may help explain how psychological state affects immune response and provide a potential mechanism for many heart and body diseases.
Rose and her team also found that blocking these neurons related to inflammation can reduce the inflammation of colitis mice. Her group hopes to apply these discoveries to humans and study the use of non -invasive brain stimuli to suppress activities to help reduce the symptoms of patients with Kroin disease and psoriasis. of. Rose said that the work is still in the early stage, "but if it can succeed, it will be very cool."
Cai's team is tracking specific neurons and circuits that regulate the immune response. In the future, she hopes to generate a comprehensive map of interaction between the brain and the immune system, outlines cells, circuits and molecular messes responsible for bidirectional communication, and associates these or physiological reading.
One of the biggest challenges is how to distinguish which cell groups have participated in these many functions. To solve this problem, some researchers have been exploring the differences in molecular levels of these cells through genetic sorting of single -cell genes. For example, this has revealed a subset of small gel cells related to neurodegenerative diseases. Stevens said how to understand how these small glue cells are different from healthy small gel cells, which will help develop the treatment. She added that these small glue cells can also be used as markers to track the progress of the disease or treatment.
Researchers have begun to use these insights on the inside and surrounding immune ecosystems. For example, Schwartz's team is trying to restore the vitality of the immune system, hoping to use this to fight Alzheimer's disease. Schwartz said that this work has opened up new ways for treatment methods, especially for neurodegenerative diseases: "This is an exciting moment in the history of brain research."
Small glue cells relieve Parkinson
Reference (click slide to view)
1.Sherwin, E., Dinan, T. G., Cryan, J. F. (2018). Recent developments in understanding the role of the gut microbiota in brain health and disease. Annals of the New York Academy of Sciences, 1420(1), 5- 25.Al of neuroscience, 40 (40), 7749-7758.
Cool brain long -term collection of brain science and psychological articles, welcome to submit


Please submit a mailbox: 2829023503@qq.com
Click here, let friends know that you love brain science
- END -
"Nine" Mi Xin!Global Internet enters "Changsha Time" again

The annual event, the Nine Mi Xin.On the morning of August 31st, the 2022 Internet...
[Directly hit the leading area] In -depth participation in local innovation!"Fipina", an open innovation project of Shiseido R & D Center, landed for the first time in China

A few days ago, Fibona, an open innovation project of Shiseido R D Center, announ...